Melanoma is an aggressive form of skin cancer that arises from pigmented cells, called melanocytes. In recent years, the incidence rate of melanoma has increased significantly, making it a public health problem of global concern. Fortunately, scientific studies have increasingly understood the molecular and genetic characteristics of melanoma, paving the way for new and promising medical therapies. This article will explore recent advances in the medical therapy of melanoma, focusing on innovative treatments such as immunotherapy, targeted therapy, and the combination of different therapeutic strategies. We will discover how these new therapeutic options are changing the clinical landscape of the disease, offering new hope and improving the survival prospects for patients affected by this serious oncological condition.
Chemotherapy: Cytotoxic drugs are used to destroy malignant cells and is administered by an oncologist. It is used in the case of local recurrences and as a treatment in advanced melanoma. The therapy can be done orally, intravenously and in case of involvement of a limb with regional perfusion.

The most used drugs are dacarbazine (DTIC, the only drug approved for the treatment of metastatic melanoma) sometimes in association with lavinblastine or cisplatin (or carboplatin) or temozolamide (orally) or fotemustine capable of determining responses in various anatomical sites and very effective on brain metastases since it is able, like temozolamide, to cross the blood-brain barrier. These drugs can also be used in combination with Tamoxifen. Temozolamide capsules have been used in some trials. Other drugs are taxanes (docetaxel, paclitaxel). Side effects obviously depend on the drugs used, but the most common are: reduction in the number of blood cells, tiredness, diarrhea, hair loss or thinning, oral ulcers, loss of fertility.
Regional perfusion
Regional Perfusion: is a method that allows drugs to remain confined to a limb without circulation in the rest of the body. It is performed in case of melanoma of the limbs and is performed under general anesthesia. The limb circulation is momentarily disconnected from the general circulation and is connected to a pump and a machine that introduces oxygen into the blood. The blood can be warmed for best results. The drug is then entered. At the end the circle is reconnected to the general circulation. Side effects are limited to mild pain, swelling and redness in the shoulder or groin, limb alopecia, rarely palmar plantar blisters
Immunotherapy: it is based on the principle that the host’s immune system is capable of generating an immune response against tumor cells. It is used in high-risk metastatic or recurrent melanoma. Currently available treatments are limited by poor response. Interferon alfa 2-b is FDA approved for the treatment of stage III melanoma with improved survival rates. It is used for one month at high doses intravenously and then subcutaneously for the following eleven months. Immunotherapy is currently the most effective treatment in the case of metastatic melanoma. The use of interleukin 2 (approved by the FDA for the treatment of stage IV melanoma) can naturally activate anti-melanoma immune cells; it is used with hospitalization and 2 cycles of high doses are performed intravenously. A study shows that out of 305 metastatic melanomas treated, 4% had complete regression and 13% had a positive response. The appearance of a “capillary leak” syndrome has limited its use, but in all ways the mortality rate induced by the use of the drug is 1%. Another drug used are the anti CTLA-4 antibodies which have given 17% of positive responses in patients with metastatic melanoma. Some patients developed severe enterocolitis and 10% complained of pituitary disorders. Other treatments used are BCG, Corynebacterium parvum and levamisole, Anti-PD-1, Anti-CD137 and Anti-CD40 antibodies. Biochemotherapy: consists of the combination of chemotherapy and interleukin 2, interferon or both.

Ipilimumab: is a monoclonal antibody studied by Bristol-Meyers Squibb and Medarex which has its target in a molecule present on T lymphocytes called CTLA-4 which blocks the body’s immune response against melanoma. Ipilimumab has been used in clinical studies in cases of metastatic melanoma also in association with dacarbazine demonstrating an extension of the life of these patients. It has been approved by the FDA for the treatment of advanced stage melanoma, only 20 or 30% of patients have a positive response (Improved Survival with Ipilimumab in Patients with Metastatic Melanoma)

Vemurafenib (Zelboraf ™): It is the second drug, after ipilimumab, to be approved for the treatment of metastatic melanoma, it blocks mutated BRAF and has a much higher rate of objectable responses, which generally occur rapidly. An attempt to use both drugs is currently underway, in fact they would appear to be able to reactivate an immune response against melanoma
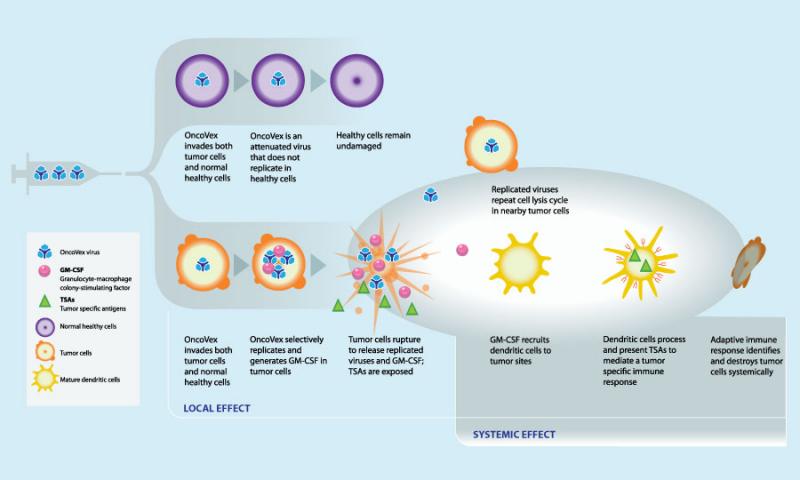
OncoVEX: a new phase 3 trial has been undertaken by the Northern California Melanoma Center with OncoVEX which is a virus which, injected into the tumor mass, enters the malignant cells and kills them without affecting the healthy cells, it is also able to produce the granulocyte macrophage colony stimulating factor which stimulates the immune response towards the tumor with clinical responses even at a distance from the injected mass. Phase 1 and phase 2 trials have yielded encouraging results with fewer side effects than Interleukin 2. Vaccination is performed every 2 weeks for a total of 24 injections or until the tumor regresses. Phase 2 results: out of 50 patients in stage IIIc (10 patients) and IV (40 patients) treated in monotherapy 10 patients had a complete response, 4 patients a partial response, 10 patients had stable disease for more than 3 months. 92% of responding patients maintained results for 7-48 months. 1-year survival was 58% and 2-year survival was 52% (results reported as of December 2009 in the Journal of Clinical Oncology).
Vaccines: currently there are no truly effective vaccines and the antitumor lymphocytes produced by active immunization have difficulty recognizing tumor cells (some vaccines are GM-CSF or GVAX).

They have been used in combination with anti CTL4 with better results. Adoptive cell transfer: autologous lymphocytes with antitumor activity are identified, stimulated in the laboratory and then increased in number and finally reinfused into patients. The results are encouraging, but the cases in which this therapy has been used are still limited. Gene therapy: two patients treated with genetically modified cells achieved significant regression in cases of metastatic melanoma. Trials currently on the course report responses around 30%.

Radiation therapy: This is usually used in the advanced stages of the disease to relieve pain or other symptoms. It is sometimes used to reduce tumor mass or in the case of bone or brain metastases. There are various therapeutic schemes which are established by a radiologist or oncologist expert in such treatment. Another radiotherapy treatment is stereotactic radiosurgery in which high doses of radiation are delivered to a specific area (Gamma Knife and CyberKnife). In the case of brain metastases, the treatment is comparable to standard radiotherapy treatment. In the case of painful bone metastases or with risk of fracture a single dose of 8Gy is used
Other therapies: the use of imiquimod 5% has been proposed in the therapy of metastatic melanoma and melanoma in situ (lentigo maligna), sometimes this treatment is proposed after surgical removal to reduce the possibility of local recurrences or satellitosis.