Nevi are proliferations of pigmentary cells, melanocytes, which aggregate assuming variable appearances. The etiological factors that favor the development of nevi are not yet fully understood, surely hormonal factors can play a role, since nevi often appear during puberty and pregnancy. Ultraviolet radiation also appears to be responsible, as nevi can often occur in areas subjected to intermittent high doses of UV.

Immunosuppression can lead to nevi (chemotherapy). The clinic of nevi can be varied, the color varies from red, red-brownish, brown, black or blue, the shape varies from round to oval and the size from a pinhead up to large dimensions (congenital nevi can affect all a limb or part of the trunk). They can be placed all over the skin and their number is variable, on average they vary from 10 to 40 nevi per person. The surface may be smooth or warty, may be flat or raised, sometimes appearing as flat lesions and then raised, rarely disappearing.

Moles can be present at birth (congenital melanocytic nevi) or they can develop later in life (acquired melanocytic nevi), although most nevi develop in the 20s. Sometimes the nevi can be surrounded by a depigmented ring in this case we speak of halo nevi or Halo nevi (Sutton nevus) often after this first phase the nevus disappears. If the whitish halo has an irregular shape, it is important to evaluate that it is not a melanoma. Giant congenital melanocytic nevi are quite rare, sometimes they can have figurative distribution assuming a “swimming trunks” arrangement, they are associated with lipomatosis or neurofibromatosis, with meningocele, spina bifida.
There have been many classifications of nevi, but the simplest distinguishes them into:
- Junctional nevi: Clusters or nests of nevi cells at the dermo-epidermal junction, tend to be flat and heavily pigmented.
- Dermal nevi: nests of nevi cells located in the dermis, often raised (sessile or papillomatous), may be highly pigmented or the same color as the skin.
- Compound nevi: Nevi cells are located both at the dermo-epidermal junction and in the dermis, sometimes appearing as raised nevi in the center and flat in the periphery.
There are also some variants of common melanocytic nevi that have clinically and histologically specific characteristics:

Blue nevus: nevus cells located deep in the dermis, appearing as a blue lesion with a dome-shaped appearance, sometimes flat. There are some variants: balloniform cells, epithelioid cells, combined (with Spitz nevus, with congenital nevus, with common nevus), compound (described by Kamino).

Spitz nevus: it was first described by Spitz in 1948 and initially defined as juvenile melanoma (Spitz S. Melanomas of childhood. Am J. Pathol 1948; 24: 591-609); it is an acquired nevus detectable mainly in children, it appears as a red-brownish, dome-shaped nodule, with a diameter often less than a centimeter, with rapid onset often present on the face or colo of children or on the trunk of adults, the dimensions vary from 1 mm to 3cm. There are some variants, sometimes the lesion can be polypoid or verrucous, other variants are Spitz nevi agminati (often grouped and distinguished in 4 variants: 1) disseminated, 2) grouped on normal skin; 3) clustered on hypopigmented skin; 4) grouped on a congenital pigmented patch). Histologically it shares many characteristics with melanoma, so the distinction is sometimes not easy; it appears to be composed of large melanocytes with large, spindle-shaped or roundish cytoplasm, with large atypical nuclei. The cells are organized in nests delimited by clear crescent fissures. We rarely have a pagetoid pseudoinfiltration resembling melanoma. The epidermis is hyperplastic and dermal inflammation is often present. Mitoses are rare. Surgical removal is recommended in adults.

Reed’s nevus: it is considered as the pigmented variant of Spitz’s nevus, it mainly affects the thorax of young adults and with dermatoscopy pseudopodia can be seen arranged around the entire contour.

Meyerson’s nevus: described by Meyerson in 1971 (he reported the case of 2 men with benign melanocytic nevi surrounded by eczema) it appears as a nevus associated with erythematous-squamous inflammation. It occurs predominantly in young adult males (3 times more frequent in males than in females). The cause is unknown and appears to be a reaction of CD4+ lymphocytes to antigens on the snow cell membrane. Both exposure to UV light and interferon alpha 2b therapy can trigger its onset. Often resolves spontaneously after a few weeks, therapy is topical with steroid creams. Excision is only advisable if a melanoma is suspected.
Recurrent nevus: it occurs after an incomplete removal of a nevus has been performed for which a melanocytic pigmentation appears in correspondence with the scar.

Becker’s nevus: Becker’s nevus is a benign lesion, often acquired during adolescence, present in all races with a prevalence in males. It appears as a usually single patch a few centimeters in diameter, brownish, often covered with hair. It occurs mainly on the shoulders, back or in the submammary area, the edges can be well demarcated, sometimes appearing irregular. The patch is asymptomatic, rare cases of itching are reported. Becker Naevus Syndrome has been described. The treatment is done for aesthetic purposes and is performed with skin removal and transplantation, with laser (cases of worsening after laser therapy to reduce pigmentation have been reported), with camouflage, electrolysis (to reduce hair).

Nevus spilus: looks like a coffee-and-milk patch dotted with multiple nevi. The dimensions can vary from a few mm to several centimeters and sometimes they are arranged metamerically. Melanomas arising on a nevus spilus have been described.
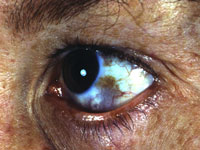
Nevus of Ota: it was first described by M.T. Ota and Tanino in 1939, appears as a bluish gray patch which is located on the first two branches of the trigeminal nerve unilaterally (bilateral cases are rare) and affects the scleral region of the eye in two thirds of cases (high risk for glaucoma); it predominantly affects females and Asian races (1 in 200 people in Japan), can be present at birth or appear during puberty. 4% of patients can develop a choroidal melanoma for which it is necessary to perform periodic checks with the ophthalmoscope. Histologically the melanocytes are present at the dermal level. It is removed with the use of Q-Switched Ruby Laser, 1064nm Q switched Nd:YAG, camouflage.

Nevus of Ito: described by Ito in 1954, it affects the shoulder and is often associated with nevus of Ota even if its incidence is lower
Nevus of Hori: it is an acquired nevus that appears with bilateral spots similar to the nevus of Ota, mainly affects oriental middle-aged women, the spots appear distinct, multiple and arranged on the cheeks, forehead, temples, eyelids and nose and progressively they tend to darken and merge. Q-switched Nd:YAG laser has been proposed as therapy
Miescher’s nevus: dome-shaped nevus of light brown colour, with a mainly smooth and regular surface which histologically affects the reticular dermis widely and is localized mainly on the face and neck and which show slow growth
Nevus of Unna: sessile nevus located mainly on the trunk and mainly affecting the papillary dermis. They often appear to have a moriform surface and have little tendency to malignant degeneration.

Sutton nevus: It is a characteristic nevus as it appears as a nevus with a circular outline without pigment. They can be single and in this case they can be secondary to trauma, or they can be multiple and in this case the dosage of thyroid hormones and anti-thyroglobulin and anti-thyroid peroxide antibodies must be performed to exclude the concomitant presence of Hashimoto’s thyroiditis. Over time, the central nevus tends to disappear and a whitish patch remains which must be well protected from the sun to avoid burns. If the amelanotic ring is rounded in most of the nevus it is benign, in some cases an irregular ring can be a sign of transformation into melanoma of the nevus. A dermatological check-up is always necessary.